This article explains the differences between typical autistic eating habits, disordered eating and eating disorders. It also advises when you should seek help from a doctor.
For relevant support services, resources and more detailed information on the topics discussed – including how to help, please click this link:
Support services and resources – autism and eating-related issues
What are eating disorders?
People with eating disorders have behaviours in relation to eating that cause significant risks to their health and / or ability to function in everyday life. Such behaviours could include not eating enough food to sustain adequate nutrition, eating too much food at once, inducing vomiting, misusing laxatives, fasting, or excessively exercising.
An eating disorder is essentially a mental illness. People with an eating disorder treat food in a way that helps them cope with difficult feelings – and can help them to feel in control. However, they may lack awareness of this. It is important to recognise that a person with an eating disorder should not be blamed for their problematic food-related habits. They deserve to be supported to recover as quickly and compassionately as possible.
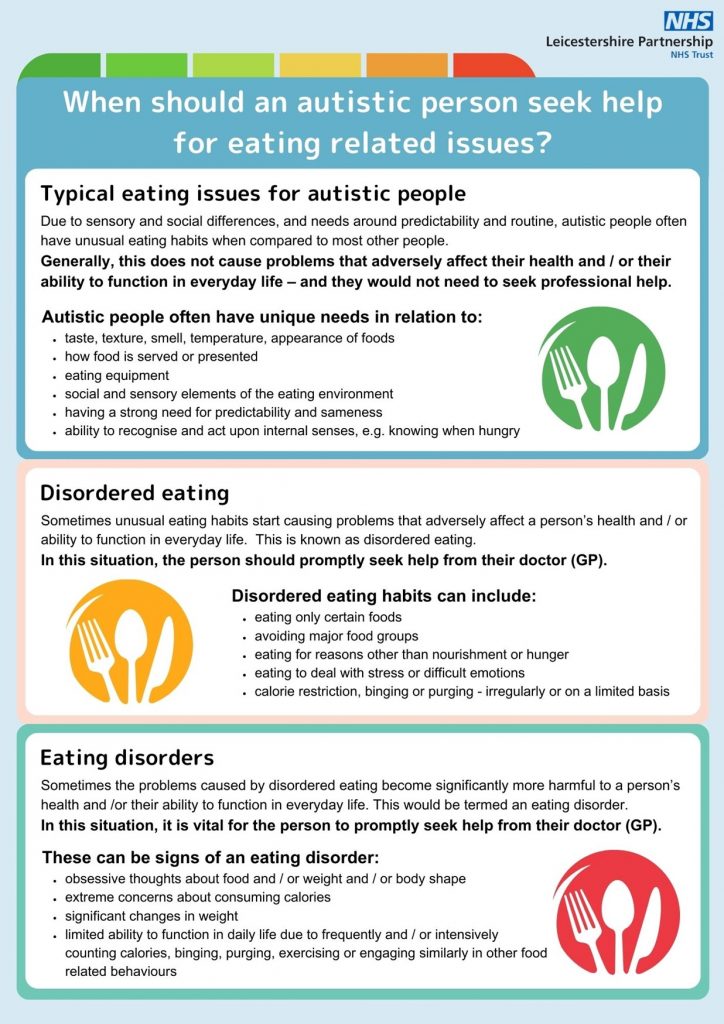
Typical autistic eating differences
This is when an autistic person has eating habits that are unusual compared to most other people – but these are not adversely affecting their health or the ability to function in daily life.
Differences in how autistic people process information, mean that each autistic person often has unique needs in relation to:
- taste, texture, smell, temperature, appearance of foods
- how food is served or presented
- eating equipment
- social and sensory elements of the eating environment
- having a strong need for predictability and sameness
- ability to recognise and act upon internal senses, e.g. knowing when hungry or full
Adapting foods and other mealtime factors to meet an autistic person’s individual needs, helps them avoid anxiety, distress and pain. It is also important to give autistic people autonomy – and to avoid stating demands and expectations.
These strategies enable them to feel regulated, i.e. comfortable, calm and safe.
The more regulated an autistic person feels, the easier it is for them to process information. This increases their ‘window of tolerance’ and makes them more likely to:
- tolerate more foods and environmental factors
- recognise when hungry and take action to eat
- plan and prepare meals and drinks
- maintain good nutrition and hydration – supporting physical and emotional health
Aspects of eating can be challenging and stressful for many autistic people.
Despite the challenges, most autistic people consume sufficient food and a broad enough range of nutrients to stay well-nourished and healthy. Therefore, they would not be considered to have disordered eating habits or an eating disorder.
However, for some autistic people, their eating related challenges can become problematic, leading to any combination of the following:
- physical health problems, e.g. unhealthy weight, digestive issues, nutritional deficiencies,
- emotional health problems, e.g. anxiety, depression, unhealthy obsessions and compulsions
- difficulty participating fully in education, work, relationships and / or social activities
It is when eating issues cause a significant impact in any of the above areas, that this is defined as either disordered eating or an eating disorder.
Why do some autistic people develop disordered eating or an eating disorder?
Information published by the National Autistic Society says non-autistic people are more likely to develop eating disorders due to issues with weight or body image perception. Whereas autistic people might develop eating disorders for different reasons such as:
- sensory differences (such as difficulty tolerating tastes and textures; difficulty recognising hunger or fullness)
- using food, calorie-counting or exercise to manage anxiety levels and /or difficult emotions – due to alexithymia
- developing an intense or obsessive interest in food, calorie-counting or exercise
- developing rules and routines around eating and exercising, that are strict and difficult to change
- excessive restrictions around food – caused by a need for control and familiarity
- feeling socially isolated and misunderstood by others – and controlling their weight in an effort to fit in and reduce social anxiety
The Peace Pathway is an organisation supporting autistic people with such problems. They have found studies indicating autistic people may be more likely to develop eating disorders due to autism-related anxieties, particularly around the social aspects of eating. A 2024 study of 180 autistic people with eating disorders highlighted that masking is the most important predictor of eating disorder symptoms in autistic people.
Types of eating disorders
There are various specific types of eating disorders, including the following:
- Anorexia Nervosa: Characterised by severe restriction of food intake, an intense fear of gaining weight, and a distorted body image
- Bulimia Nervosa: Involves cycles of binge eating followed by compensatory behaviours such as vomiting, excessive exercise, or laxative use
- Binge Eating Disorder (BED): Marked by recurrent episodes of eating large quantities of food, often quickly and to the point of discomfort, without regular use of compensatory behaviours
- Rumination Disorder: Involves regurgitating food that has been previously swallowed, which is then re-chewed, re-swallowed, or spit out
- Other Specified Feeding or Eating Disorder (OSFED): Includes eating disorders that don’t fit the criteria for the other specific disorders but still cause significant distress or impairment
- Orthorexiais characterised by an unhealthy obsession with eating foods that the person considers healthy or “pure.” It is not currently formally recognised as an eating disorder. However, if a person is suffering with their emotional and / or physical health and it is suspected that this could be in relation to orthorexia, help should be sought from their doctor.
- ARFID
- Pica
ARFID and pica warrant a more detailed explanation as they are both eating disorders, that autistic people may be particularly more prone to than non-autistic people.
What is ARFID?
ARFID is the abbreviated term for avoidant and restrictive food intake disorder. Here is the UK it is recognised as an eating disorder.
According to UK charity ARFID awareness, ‘ARFID is more than just ‘picky eating’. It is characterised by a pattern of eating that avoids certain foods or food groups entirely and/or is restricted in quantity (eating small amounts). It is not due to lack of available food, or cultural norms (e.g. someone who is fasting or chooses not to eat certain foods for religious or cultural reasons alone)’.
ARFID can be caused by hypersensitivity to textures and / or tastes, which is a common feature in autistic people. As with all other eating disorders, when compared to the non-autistic population, autistic people have a higher than usual risk of developing ARFID. However, whilst many autistic people have a limited range of foods they can tolerate in terms of taste, texture and / or smell – if they are able to eat at least 10 types of food items, they would not be given an ARFID diagnosis.
ARFID can also be caused by a phobia, such as a fear of having an allergic reaction or choking – which could be due to a past traumatic experience.
What is pica?
Pica is an eating disorder where the person eats non-food items that have no nutritional value. Pica can affect anyone, though when compared to the general population, it is more common for autistic people. Every person with pica is different in terms of what substances they eat. Possible pica items could include: paper, ice, chalk, dirt, plastic, hair.
Research has yet to confirm why people develop pica. It is likely that the causes vary from person to person. They might include: not realising the difference between foods and non-foods; a need for sensory feedback; anxiety relief; to avoid a demand; to gain attention.
Although pica is unusual – it is not always harmful, as most people with pica also eat regular food and get sufficient nutrition. And some people with pica eat non-food items that are effectively harmless.
However, in some cases, people with pica might eat materials that cause serious health issues – such as poisoning, infections or digestive blockages. It is often such health issues that lead to previously unrecognised pica being discovered.
When a person has pica it is important to try and understand as much as possible about pica, what might be driving the person to eat non-food stuffs – what strategies to try to help reduce risk.
To get a pica diagnosis, the behaviour must have persisted for at least one month and not be part of a cultural practice. Pica diagnoses are not usually given to children under two. This is because babies and toddlers often ‘mouth’ non-food items as part of their normal development – and sometimes these are accidentally consumed.
If you’re concerned about yourself or someone else, you should visit your doctor as quickly as possible so that they can refer you for appropriate treatment.
When to seek help
It’s vital to know the signs of disordered eating or an eating disorder so that you can seek help quickly and reduce the risk of harm.
BEAT eating disorder charity have created a tips campaign to help you recognise the eating disorders where there tend to be an underlying, unhealthy fixation with weight and / or body shape and / or health
Here’s what they say you should look out for:
- Lips – Are they obsessive about food?
- Flips – Is their behaviour changing?
- Hips – Do they have distorted beliefs about their body size?
- Kips – Are they often tired or struggling to concentrate?
- Nips – Do they disappear to the toilet after meals?
- Skips – Have they started exercising excessively?
The signs of ARFID or pica are different. As autistic people can be prone to these conditions, it is important to familiarise yourself with the behaviours and risks associated with them.
if a person has unusual eating related habits and these coincide with ill health, being excessively underweight or overweight, you should suspect they could be suffering from disordered eating or an eating disorder. You should also suspect this if their eating habits make it difficult or stressful for a person to take part in everyday life, such as attending school or work, socialising and / or being able to take care of their own basic needs.
If you suspect you or someone you care about might have disordered eating or an eating disorder, you must seek help from a doctor (GP) as quickly as possible. This ensures the best possible chance of full recovery.
What to expect when you visit the doctor (GP) about possible disordered eating or an eating disorder?
It can be helpful to plan before you have your appointment. Write down your symptoms and your concerns. Consider taking someone with you for support and to help you remember what to say and what to ask.
The doctor (GP) will ask questions, in relation to the person’s eating – and their mental and physical health. Topics they will need to find out about:
- the person’s eating related habits – such as restricting intake, purging, binging or excessive exercise
- if the person has any food / eating related stresses, fears, sensory aversions or compulsions
- if the person has any excessive, obsessive and / or irrational concerns about their weight and / or body shape and / or health and fitness
- if the person has any emotional and / or physical health issues
To help you remember this information, you could keep an eating habits diary for a short while.
Your doctor should also check your weight and may also need to do blood tests to check your physical health.
If a GP suspects you could have an eating disorder, they will refer you to a specialist eating disorders service. However, as GPs are not eating disorders specialists, they might not be clear about when it is necessary to make a referral.
If you have any concerns that you have not been listened to or well supported – or that a referral was not made when you feel it should have been, you can:
- ask for another appointment with a different GP
- contact BEAT eating disorders charity helpline and ask for their advice
If you are worried that you or your loved one might have an eating disorder, you need to be sure your concerns have been fully understood and addressed. Do not give up until this has happened – because with eating disorders, it’s important to get help as soon as possible.
If you are referred to a specialist eating disorders service, you may feel scared about what to expect. Be assured that this is normal and that people working in these services are empathic and experienced in supporting people with eating disorders who are feeling highly anxious. You may wish to seek support from a specialist helpline such as BEAT as they can help you learn about what to expect and give you tips on how to best cope.
You may have to wait a few weeks before you get a letter telling you about your first appointment. Whilst you wait for this appointment, if you have any concerns about your mental or physical health, you should talk to your GP.
If you have an eating disorders assessment, you may need treatment. Types of treatment vary and depend on individual circumstances and needs. The NICE Guidelines for Eating Disorders gives an idea of some the different possible types of treatments.
In summary:
Most autistic people have eating related challenges and eating habits that can be considered unusual when compared to those of neurotypical people. Despite these challenges, their health or ability to function well in their daily lives in not usually negatively affected.
However, some autistic people have eating related habits and challenges that cause problems with their mental and / or physical health. These problems may also affect their ability to function in daily life.
When this happens, the person should talk to their doctor as soon as possible, as they may need a referral to a specialist eating disorders team. This team can carry out an assessment and give them treatment tailored to meet their individual needs.
When a person is given timely support for their eating disorder, they have the best chance of gaining full recovery.
____________________________________________________________________________________________________________________________________________________________________
For our directory of eating related resources and services, please click here
___________________________________________________________________________________________________________________________________________________________________________________
Sources
Camouflaging is the most important predictor of eating disorder symptoms in autistic people
Studies showing the connection between ARFID and autism
Frontiers | Estimating the Prevalence and Genetic Risk Mechanisms of ARFID in a Large Autism Cohort
ARFID is more than ‘picky eating’
A study about living with ARFID via analysis of online blogging